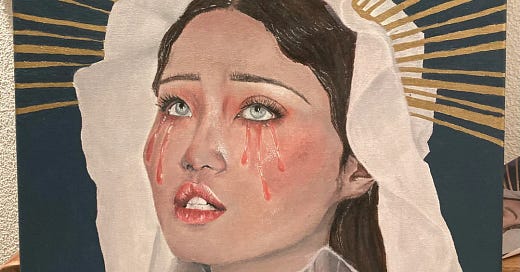
🩸 “Iron Deficiency” or Iron Misunderstood?
Rethinking Anemia, Oxidative Stress, and the Silent Load Women Carry
By Mauve Paper
Iron is often offered to women like an apology — for the blood we lose, the fatigue we feel, the fog we carry through our cycles. A pill to patch a deficiency. A bottle to boost a low.
But what if the story is incomplete?
What if “low iron” isn’t always a shortage — but a misplacement?
What if our bodies aren’t iron-depleted, but iron-distressed?
And what if the rising tide of anemia isn’t solved by more — but by understanding why the body hides iron in the first place?
This is not an argument against the existence of true anemia. This is an invitation to question how we define it, treat it, and live with its shadow.
📖 Part I — The Weight of Iron
Iron is a paradox. We need it for oxygen delivery, mitochondrial energy production, and enzymatic reactions. But it’s also biochemically aggressive — a transition metal that, when left unbound, catalyzes free radical formation via the Fenton reaction, triggering oxidative damage to lipids, proteins, and DNA.
“Excess iron is a crucial element in transforming stress into tissue damage.” — Ray Peat
Iron doesn’t float freely in the body by accident. It's kept bound tightly to ferritin, transferrin, ceruloplasmin, or locked within red blood cells. The moment it escapes? It becomes a biological arsonist.
And yet, we casually ingest it in fortified cereals, prenatal pills, and multivitamins — trusting that more is safer.
But is it?
🧬 Part II — Anemia Isn’t Always a Deficiency
We are told we are iron-deficient based on lab results: low ferritin, low hemoglobin, or borderline hematocrit. But many women who present as “anemic” are not actually low in total iron — they’re unable to use or move it.
Iron can be present in the body but:
Trapped in tissues due to inflammation
Unusable due to copper deficiency or low ceruloplasmin
Locked inside ferritin, not available for red blood cell synthesis
This creates a functional anemia — not from lack, but from misallocation.
Think of it as a warehouse full of supplies, but no shipping trucks to move them.
🔁 Part III — Iron and the Inflammatory Loop
Here’s how iron toxicity can mimic deficiency:
Inflammation (gut infections, stress, endotoxemia) releases hepcidin, blocking iron export from cells.
Iron becomes trapped in macrophages and hepatocytes.
Blood levels drop, but tissues become overloaded.
Supplementing adds more iron to an already flooded system, increasing oxidative stress.
Over time, this leads to:
Liver iron buildup
Pancreatic damage
Mitochondrial injury
Neuroinflammation
This is not a rare event. It’s a modern pattern — especially in women under chronic stress, with estrogen dominance, or on hormonal contraception.
🧠 Part IV — Iron and Estrogen: The Feminine Crossfire
Estrogen increases iron absorption. It also:
Suppresses thyroid activity
Enhances histamine responses
Promotes copper loss
This makes the female body uniquely vulnerable to iron mismanagement. A woman with high estrogen, low thyroid, and marginal copper will store iron ineffectively — raising oxidative stress without solving fatigue.
It’s no surprise that these same women:
Have dark under-eyes (subcutaneous iron)
Bruise easily (capillary fragility)
Feel tired despite supplements
Their mitochondria are inflamed, not malnourished.
🌍 Part V — Iron Fortification: A Modern Health Crisis?
Ray Peat points out a disturbing shift: since the 1940s, iron fortification in food has exploded — especially in grains, cereals, and flour. This happened with little consideration for absorption dynamics or metabolic individuality.
We now eat iron:
In flour that’s baked, oxidized, and stripped of cofactors
In meat raised on inflammatory soy
In prenatal pills that overload mothers without testing for copper, zinc, or ferritin saturation
Even infants are fed iron-fortified formula, priming their liver and brain for early oxidative stress. Studies show excess neonatal iron is linked to:
Cognitive decline
Autism risk
Early tissue calcification
What Ray Peat Advocated Instead
Ray Peat’s approach was never anti-nutrient — it was pro-context. His suggestions for iron regulation include:
🍖 1. Eat Real Iron Sources
Shellfish, liver, and red meat contain heme iron, which is better regulated by the body than synthetic forms.
Avoid non-heme iron in cereals, fortified flours, and pills unless absolutely necessary.
🧈 2. Support Metabolic Flow
Ensure good thyroid function (T3/T4 balance) to enable iron use.
Protect the liver with saturated fats and cholesterol-rich foods.
🥣 3. Minimize Iron Absorption When Not Needed
Drink coffee or tea with iron-rich meals (tannins reduce absorption).
Avoid taking vitamin C with high-iron meals unless deficiency is confirmed.
🧂 4. Respect Cofactors
Iron cannot be used well without copper, vitamin A, and retinol.
Favor natural sources of these (liver, oysters, egg yolks).
Reclaiming Energy Without Iron Overload
If you’ve been told to take iron, pause and ask:
Have you checked ferritin, serum iron, TIBC, transferrin saturation, and CRP?
Have you evaluated thyroid, copper, and zinc status?
Are you losing blood excessively or are you under metabolic stress?
Fatigue can be from:
Low thyroid, not low iron
Low sodium, not anemia
Mitochondrial damage, not nutrient lack
If iron is flooding tissues while staying low in blood, more iron is not the answer — removing the block is.
🪶 Final Words: A Softer Look at Anemia
Women live in cycles. We bleed. We rebuild. But not all fatigue is a failure. Sometimes, it’s a signal — that the system is overwhelmed, not empty.
We don’t always need more. Sometimes we need to use what we already have — better.
At Mauve Paper, we believe the most powerful form of nourishment isn’t force — it’s alignment. Listen to your labs, yes — but also listen to your story.
Let’s stop confusing iron as energy when what we really need is clarity, oxygen, and rest.
Mauve Paper is a space for metabolic literacy, hormonal nuance, and biological beauty. If this post expanded your view, consider subscribing. We're building a future where women ask better questions — and receive better answers.